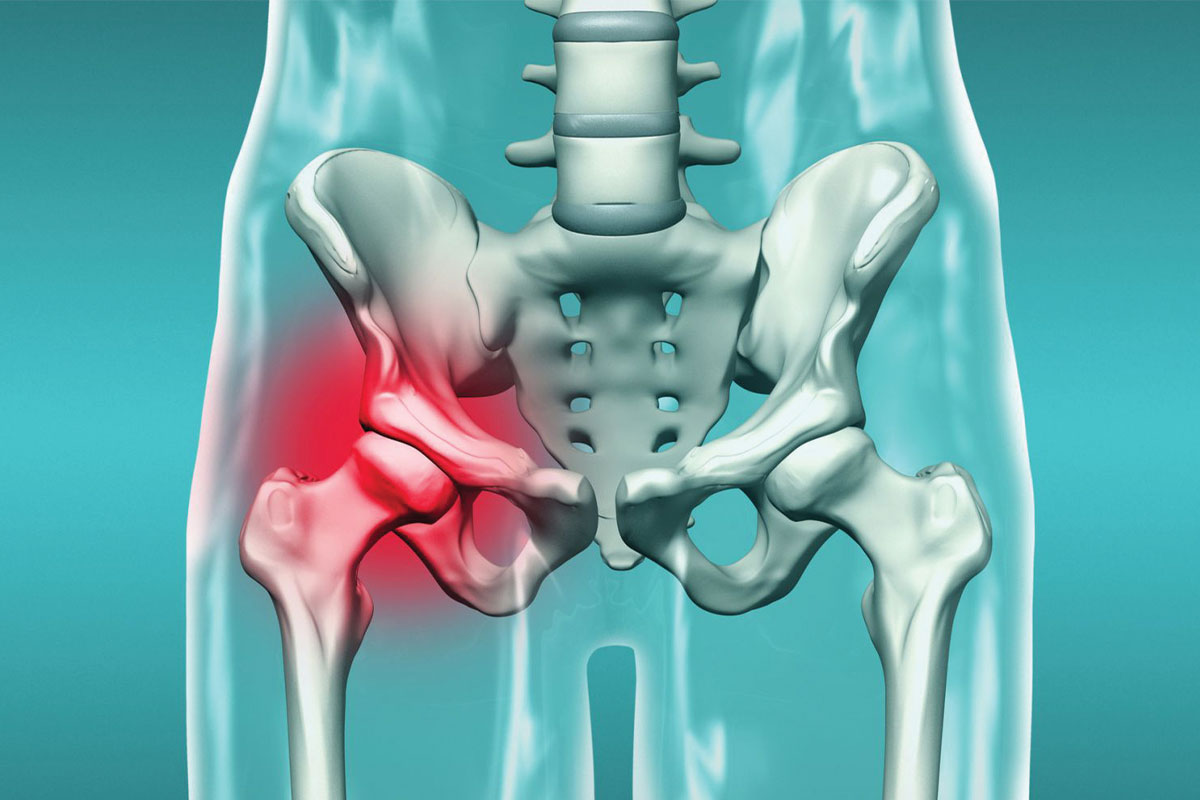
The condition known as hip dislocation is actually referred to as developmental hip dysplasia (DHD) in medical terminology today. Developmental hip dysplasia (DHD) is a condition where the hip joint does not develop properly, leading to instability or dislocations in the joint. It can range from mild instability (looseness) to complete dislocation. This condition is more common in infants and may occur during fetal development or within the first few months after birth.
Hip dysplasia can be caused by various factors, including genetic predisposition, breech position in the womb, and other environmental factors. It is more common in females and firstborn children. If left untreated, it can lead to walking problems, hip pain, and osteoarthritis (joint degeneration) in later life. Hip dislocation is one of the leading causes of preventable or correctable limping.
Early diagnosis and treatment are crucial for better outcomes. Treatment options may include the use of a special device or brace to keep the hip joint in place or, in severe cases, surgery to correct the position of the hip joint.
What Are the Symptoms of Hip Dislocation?
Developmental hip dysplasia (DHD), also known as hip dislocation, can manifest with various symptoms depending on the severity of the condition. Some common signs and symptoms associated with DHD include:
Loss of movement in the hip joint: This can often be noticed when changing diapers in babies, where one leg may be harder to open than the other. In cases of bilateral dislocation, it may be difficult for caregivers to detect.
Asymmetrical thigh or gluteal (buttock) folds where one side appears higher or fuller than the other: Differences in the folds at the back of the legs can be a sign of hip dislocation, although this alone may not confirm the diagnosis as asymmetry can sometimes be normal.
Clicking or popping sensation in the hip joint during movement: This is often associated with the ability of the examining doctor to easily dislocate and reposition the hip joint. In some cases, caregivers may also notice this.
Unequal leg lengths, where one leg appears shorter than the other: In unilateral dislocations, differences in leg length can be detected by caregivers, especially before the child reaches one year of age, due to the higher placement of the dislocated hip.
In severe cases, complete dislocation of the hip joint can cause the affected leg to appear shorter and more outwardly rotated compared to the unaffected side: This is more pronounced in children with a significant limp when they start walking.
It is important to note that some babies with hip dislocation, especially milder cases, may not show any noticeable symptoms. Therefore, regular physical examinations by an orthopedic doctor are crucial for early detection and appropriate treatment of developmental hip dysplasia. Additionally, imaging studies such as ultrasound or X-rays may be requested to confirm the diagnosis and assess the severity of the condition.
Ultrasound in Hip Dislocation Diagnosis
Ultrasound is a commonly used imaging method for diagnosing developmental hip dysplasia (DHD) in infants.
Ultrasound is typically performed when there are clinical signs or risk factors for DHD, such as breech presentation at birth, a family history of hip dysplasia, or abnormal physical examination findings (e.g., limited hip abduction, asymmetrical thigh or gluteal folds). In countries like Turkey, where hip dislocation is common, it is also included in routine screening programs.
Evaluation of the Hip Joint: An ultrasound probe is placed over the hip joint to obtain images that assess the structure and stability of the joint.
Ultrasound provides measurements of various parameters, such as the alpha angle and acetabular depth-to-width ratio, which are used to evaluate the severity of hip dysplasia. The alpha angle measures the relationship between the femoral head (the ball of the hip joint) and the acetabulum (the socket of the hip joint). In normal hips, the alpha angle is typically greater than 60 degrees, indicating a well-formed and aligned hip joint. A decreased alpha angle (<60 degrees) suggests hip dysplasia or dislocation.
The diagnosis of congenital hip dislocation (developmental hip dysplasia) can be easily and painlessly made through ultrasound screening. Hip ultrasound screening in infants is usually performed between the first and second months after birth. Since ultrasound uses sound waves, it poses no harm to the child. After six months, as the hip bones begin to mature, ultrasound may not provide enough information, and X-rays taken in the frog-leg position are used for diagnosis in children older than six months.
Hip Dislocation and Swaddling
While swaddling has its benefits, it’s essential to ensure that the baby’s hips have enough room for healthy development. Excessively tight swaddling or incorrect positioning can increase the risk of developmental hip dysplasia (DHD). A safe swaddling technique involves allowing the baby’s legs to bend and move freely at the hips. While there is no known harm in swaddling the arms tightly, the hip area should be swaddled loosely.
Hip Dislocation and Pavlik Harness
The Pavlik harness is a commonly used device for treating developmental hip dysplasia (DHD) in infants. It is the most important treatment option for early-detected cases where the hip can be repositioned without the need for surgery.
The Pavlik harness is designed to hold the hip joint in a position that supports proper development while allowing natural movement and growth. It is used in infants with mild to moderate DHD, where the hip joint can still be reduced (returned to the socket) without requiring surgery.
The Pavlik harness consists of soft fabric straps and adjustable buckles that secure around the baby’s chest, shoulders, and legs. The harness includes padded shoulder straps, a waist belt, and foot stirrups that help position the hips correctly. The harness can be adjusted to accommodate the baby’s growth and is custom-fitted to ensure comfort. Therefore, the use of the Pavlik harness poses no risk related to the child’s growth.
The Pavlik harness is applied after the orthopedic physician reduces the hips into the socket, and the straps are secured in the correct position. It is recommended to mark the straps with a pen to ensure they stay in place after positioning.
During harness application, the baby is positioned on their back (lying on their back). The straps are adjusted to keep the hips in the correct position, with the knees bent and the hips opened outward. The straps are secured tightly but not too tight, allowing for proper circulation and movement.
The duration of Pavlik harness treatment depends on the severity of DHD and the response to treatment.
Infants wear the harness full-time (23 hours a day), with short breaks for bathing and skincare. Frequent removal of the harness and breaks in treatment are not recommended.
Follow-up is recommended at least every three weeks during treatment to assess hip development and ensure proper application. Depending on the child’s age, follow-up may include ultrasound or X-ray monitoring.
Special attention should be given to maintaining skin hygiene, monitoring for signs of skin irritation or redness, and ensuring the harness straps remain securely fastened.
Once the hip joint stabilizes and imaging studies show satisfactory hip development, the Pavlik harness treatment can be discontinued. The orthopedic physician will determine when it is appropriate to stop using the harness based on clinical and radiographic evaluations.
After Pavlik harness treatment, ongoing monitoring may be necessary to ensure stable hip development and to evaluate for any residual hip dysplasia or related issues. Even if the hip joint has been successfully repositioned and adequate development has occurred with the harness, follow-up should continue periodically until the child is 15 years old.
Overall, the Pavlik harness is an effective, non-invasive treatment option for infants with DHD. It promotes proper hip development and reduces the need for surgery in many cases. However, successful outcomes depend on early diagnosis, proper harness application, careful monitoring, and adherence to treatment protocols. Parents and caregivers play a crucial role in supporting their baby’s treatment journey by following the orthopedic physician’s recommendations and participating in ongoing care and follow-up.
Surgical Treatment Methods for Hip Dislocation
Surgical intervention for developmental hip dysplasia (DHD) is typically considered when conservative treatments like harnesses or casting do not provide sufficient hip joint stability or fail to reduce hip dysplasia. Surgical interventions aim to reposition and stabilize the hip joint, support proper development of the hip socket (acetabulum), and address any problems associated with DHD. These procedures range from soft tissue adjustments to correcting bone structures and reshaping the hip socket.
Open Reduction With or Without Pelvic Osteotomy:
Open reduction is often considered for infants with severe hip dysplasia or dislocation that cannot be adequately treated with non-surgical methods. During open reduction, the surgeon makes an incision to directly access the hip joint. The femoral head is repositioned within the acetabulum, and any soft tissue barriers preventing reduction are removed. In some cases, additional procedures such as pelvic osteotomy (reshaping the bones of the pelvis) may be performed to improve femoral head coverage by reshaping the acetabulum.
Closed Reduction With or Without Arthrography:
Closed reduction is a less invasive alternative to open reduction for infants with less severe hip dysplasia. It may also be considered as a salvage procedure if open reduction fails. Closed reduction involves manipulating the hip joint without making an incision to reposition the femoral head within the acetabulum. Fluoroscopy or ultrasound guidance (arthrography) may be used to assist in achieving proper reduction. After successful closed reduction, a cast may be applied to immobilize the hip and allow for healing. The duration of cast immobilization depends on factors such as age, severity of dysplasia, and stability of the reduction.
Following surgical intervention, close monitoring of the hip joint is essential to evaluate proper healing, joint stability, and range of motion. Physical therapy may be initiated to support muscle strength, joint mobility, and motor development. In some cases, additional follow-up surgeries may be needed to maintain optimal hip function and address any residual issues related to DHD. Follow-up imaging studies are performed regularly to assess hip joint development and detect any potential complications.
Possible Problems in Hip Dislocation Follow-Up
Potential issues associated with the surgical treatment of developmental hip dysplasia (DHD) include infection, avascular necrosis of the femoral head, redislocation, and leg length discrepancies. Careful preoperative planning, meticulous surgical technique, and proper postoperative management are essential to minimize the risk of these problems and optimize outcomes.
The success of surgical treatment for DHD depends on various factors, such as the severity of the dysplasia, the child’s age at the time of intervention, the surgical technique used, and postoperative management. Early diagnosis and intervention, combined with comprehensive multidisciplinary care, can lead to positive outcomes, including improved hip joint stability, function, and long-term joint health.
Family Education in Hip Dislocation:
Family education is a critical component of the surgical treatment of DHD. Since the patients in this group are children and most cannot manage their own care, family education is essential. Parents should be informed about the nature of the condition, treatment options, the potential risks and benefits of surgery, and what to expect during postoperative recovery and rehabilitation.
Clear communication with the healthcare team and active participation in decision-making can help achieve the best outcomes and patient satisfaction.
It’s important to note that the specific surgical approach and techniques used may vary depending on individual patient factors, the preferences of the physician, and the experience of the surgeon. Therefore, the decision to pursue surgical intervention for DHD should be made in consultation with a multidisciplinary team of healthcare professionals, including orthopedic surgeons, radiologists, physical therapists, and pediatric specialists, to tailor the treatment.
Frequently Asked Questions
What are the signs and symptoms of developmental hip dysplasia (DHD)?
Symptoms of DHD include limited range of motion in the hip joint, asymmetrical thigh or gluteal folds, a clicking or popping sensation in the hip, unequal leg lengths, and a preference for one leg over the other when crawling or walking.
How is developmental hip dysplasia diagnosed?
DHD is typically diagnosed through a combination of physical examination, including the Ortolani and Barlow tests, and imaging studies such as ultrasound or X-ray to assess hip joint morphology and stability.
When should a child be screened for developmental hip dysplasia?
Screening for DHD is usually performed between the first and second months after birth as part of routine newborn checkups.
What are the treatment options for developmental hip dysplasia?
Treatment depends on the severity of the condition and the child’s age. Options include observation, the use of a Pavlik harness to hold the hip in place, or surgical interventions such as closed or open reduction, with or without osteotomy.
How does the Pavlik harness work, and how long is it worn each day?
The Pavlik harness is a device used to keep the hip joint in a stable position, allowing for proper alignment and development. It is usually worn full-time, 24 hours a day, for several weeks to months, depending on the severity of hip dysplasia and the child’s response to treatment.
What are the potential complications of untreated developmental hip dysplasia?
If left untreated, DHD can lead to walking difficulties, hip pain, and osteoarthritis in later life. Severe cases can cause permanent deformity and functional impairment of the hip joint. Unilateral shortening can eventually result in spinal curvature and scoliosis.
What is the prognosis for children with developmental hip dysplasia?
With early diagnosis and appropriate treatment, the prognosis for children with DHD is generally favorable. However, outcomes can vary depending on the severity of the condition and the effectiveness of the treatment.
Can developmental hip dysplasia be prevented?
While some risk factors for DHD, such as breech presentation, cannot be prevented, early screening and intervention can help reduce the severity of the condition and minimize long-term complications. Early use of harnesses or simpler surgical procedures can lead to good long-term results.